- Full Guideline (this review references this booklet)
- Patient Guideline
- Quick Reference Guide
- Costs and Resources to implement in Scotland
Coronary Heart Disease (CHD) is a disease of the heart and coronary arteries caused by a build of fatty materials in the blood vessels which supply the heart with oxygen. This can cause a heart attack, or chest pain or angina.
My risk of CVD in the next 10 years is 1 in 12.5 (8%) according to my 'ASSIGN' score (table 1). So for every 1000 persons with my CVD risk, 80 will have a CVD event in the next 10 years.
Other Factors - not accounted for by 'ASSIGN' score
- At 102cm I have borderline abdominal obesity (defined as greater or equal to 102cm waist measurement in men). (4.7 pg 15)
- waist hip ratio is 102cm/98cm = 1.04 (<0.95>
- I'm overweight BMI >25 (12st 6 pounds, height 5'7.5", BMI 27.5).
In October 2006 my blood tests were:
- 5.1 mmol/l total cholesterol (NHS normal: <=5.0)
- 3.0 mmol/l LDL 'bad' cholesterol
- 1.02 mmol/l HDL 'good' cholesterol (normal >1.03) (4.7 pg 15)
- total cholesterol/HDL cholesterol ratio = 5.0
- Blood pressure = 130 systolic/70 diastolic (normal <130/85)
- On 30th April 2007 my figure (ex Poole Hospital 110/70)
- 5.9 mmol /l glucose
 The report defines people in a 'High Risk' category if they have a >=20% risk of CVD over the next 10 years. For those with 1% annual risk of CVD ( viz. 10% over 10 years) benefits have been shown using statins (3-Hydroxy-3-Methylglutaryl-CoA (HMG-CoA) Reductase inhibitors). Annual CVD is 1% in USA and Europe. So most middle aged men and women could benefit from a statin and CVD reduction. (Full Guideline (FG) 2.4 pg 11) 8.2 Aspirin Antiplatelet therapy with Aspirin reduces Myocardial Infarction (heart attack) risk but increases stroke and major gastrointestinal bleeding risk. P S Sanmuganathan et al in Heart85:265-271 2001; concluded "Aspirin treatment for primary prevention is safe and worthwhile at coronary event risk greater than 1.5%/year; safe but of limited value at coronary risk 1%/year; and unsafe at coronary event risk 0.5%/year." With my 8% over 10 year CVD risk, Aspirin is of limited value or unsafe. 9 Lipid Lowering Low density Lipoprotein (LDL) makes up 60-70% of serum cholesterol. The Friedwald equation LDL = TC-HDL-(TG/2.2) (9.2 pg 32) Statins reduce Total Cholesterol TC by approx. 20% or 1mmol and LDL Cholesterol by 30% (9.3, pg 28) with a 30% reduction in CHD mortality (9.3 pg 29).
The report defines people in a 'High Risk' category if they have a >=20% risk of CVD over the next 10 years. For those with 1% annual risk of CVD ( viz. 10% over 10 years) benefits have been shown using statins (3-Hydroxy-3-Methylglutaryl-CoA (HMG-CoA) Reductase inhibitors). Annual CVD is 1% in USA and Europe. So most middle aged men and women could benefit from a statin and CVD reduction. (Full Guideline (FG) 2.4 pg 11) 8.2 Aspirin Antiplatelet therapy with Aspirin reduces Myocardial Infarction (heart attack) risk but increases stroke and major gastrointestinal bleeding risk. P S Sanmuganathan et al in Heart85:265-271 2001; concluded "Aspirin treatment for primary prevention is safe and worthwhile at coronary event risk greater than 1.5%/year; safe but of limited value at coronary risk 1%/year; and unsafe at coronary event risk 0.5%/year." With my 8% over 10 year CVD risk, Aspirin is of limited value or unsafe. 9 Lipid Lowering Low density Lipoprotein (LDL) makes up 60-70% of serum cholesterol. The Friedwald equation LDL = TC-HDL-(TG/2.2) (9.2 pg 32) Statins reduce Total Cholesterol TC by approx. 20% or 1mmol and LDL Cholesterol by 30% (9.3, pg 28) with a 30% reduction in CHD mortality (9.3 pg 29). 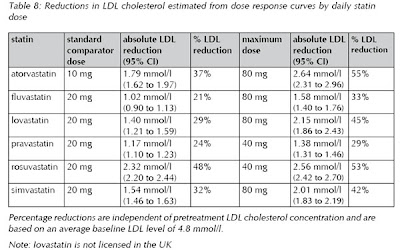 With each doubling of the dose of a statin LDL levels fall by 6%. A reduction of 1.6 mmol/l halves the risk of CHD events after 2 years and this reduction can be achieved with standard doses of statins. (9.4 pg 30, table 8) My 8% (1 in 12.5) risk of CVD (table 1, total cholesterol 5.1 mmol/l) could be reduced to a 6% risk (1 in 17) (table 2, total cholesterol 3.88 mmol/l) - a 25% risk reduction. 80 people per thousand, like me, will have CardioVascular Disease over 10 years. By taking Statins that risk is reduced to 60 people with CVD. Mild muscle pains or other adverse effects (eg fever, malaise) may require reduction in statin levels or change of statin type whilst severe side effects will require statin therapy to be discontinued. (para 9.6, pg 36). Current NHS target for individuals at high cardiovascular risk is a TC level of less than 5 mmol. Reducing this target to 4.5 or 4.0 mmol/l would have major resource implications for NHS (9.7 pg 32). Zocor (simvastatin, 10mg per day) is available from Boots over the counter for £8 per month. HDL Cholesterol my level of 1.02 mmol/l HDL Cholesterol is low and may require treatment with Fibrates (raises levels 10-15%,) (9.10.2 pg 39) or Nicotinic Acid (raises levels 15-35%) (9.10.3 pg 40) 9.8 Safety of Statins Statins are safe. No increase in cancer levels has been found. Raised levels of liver enzymes (aspartate and alanine aminotransferase) occur in 1% cases which is completely reversible when treatment is withdrawn. Minor muscle discomfort is common though the incidence varies. Rare more serious Myopathy with raised creatine kinase occurs in 0.1% cases. In 0.01% cases Rhabdomyalysis (renal failure) occurs. Withdrawal of treatment leads to recovery in a majority of cases but death can occur if patient is receiving several drug treatments or experiencing multiple symptoms. Statins may possibly interact with other medications eg fibrates (niacin, nicotinic acid). Inhibitors of cytochrome P450 and grapefruit juice may increase Myopathy risk. Atorvastatin, fluvastatin, pravastatin, rosuvastatin and simvastatin are licensed for use in UK. Annex 2 pg 62 Joint British Societies (JBS2 - reference 28) proposed total cholesterol target of <4mmol/l size="4">Annex 3 pg 65 Creatine Kinase (CK) baseline pretreatment level might be useful to monitor possible muscular symptoms. Annex 4 pg 66 Liver transaminase levels advisable prior to statin treatment, 3 months after treatment and when dose level is increased. This indicates potential for jaundice, malaise, fatigue, lethargy etc. Annex 5 pg 67 Assessment of renal function is advisable before starting statin therapy. Test for serum creatinine and proteinuria. Conclusions for my health
With each doubling of the dose of a statin LDL levels fall by 6%. A reduction of 1.6 mmol/l halves the risk of CHD events after 2 years and this reduction can be achieved with standard doses of statins. (9.4 pg 30, table 8) My 8% (1 in 12.5) risk of CVD (table 1, total cholesterol 5.1 mmol/l) could be reduced to a 6% risk (1 in 17) (table 2, total cholesterol 3.88 mmol/l) - a 25% risk reduction. 80 people per thousand, like me, will have CardioVascular Disease over 10 years. By taking Statins that risk is reduced to 60 people with CVD. Mild muscle pains or other adverse effects (eg fever, malaise) may require reduction in statin levels or change of statin type whilst severe side effects will require statin therapy to be discontinued. (para 9.6, pg 36). Current NHS target for individuals at high cardiovascular risk is a TC level of less than 5 mmol. Reducing this target to 4.5 or 4.0 mmol/l would have major resource implications for NHS (9.7 pg 32). Zocor (simvastatin, 10mg per day) is available from Boots over the counter for £8 per month. HDL Cholesterol my level of 1.02 mmol/l HDL Cholesterol is low and may require treatment with Fibrates (raises levels 10-15%,) (9.10.2 pg 39) or Nicotinic Acid (raises levels 15-35%) (9.10.3 pg 40) 9.8 Safety of Statins Statins are safe. No increase in cancer levels has been found. Raised levels of liver enzymes (aspartate and alanine aminotransferase) occur in 1% cases which is completely reversible when treatment is withdrawn. Minor muscle discomfort is common though the incidence varies. Rare more serious Myopathy with raised creatine kinase occurs in 0.1% cases. In 0.01% cases Rhabdomyalysis (renal failure) occurs. Withdrawal of treatment leads to recovery in a majority of cases but death can occur if patient is receiving several drug treatments or experiencing multiple symptoms. Statins may possibly interact with other medications eg fibrates (niacin, nicotinic acid). Inhibitors of cytochrome P450 and grapefruit juice may increase Myopathy risk. Atorvastatin, fluvastatin, pravastatin, rosuvastatin and simvastatin are licensed for use in UK. Annex 2 pg 62 Joint British Societies (JBS2 - reference 28) proposed total cholesterol target of <4mmol/l size="4">Annex 3 pg 65 Creatine Kinase (CK) baseline pretreatment level might be useful to monitor possible muscular symptoms. Annex 4 pg 66 Liver transaminase levels advisable prior to statin treatment, 3 months after treatment and when dose level is increased. This indicates potential for jaundice, malaise, fatigue, lethargy etc. Annex 5 pg 67 Assessment of renal function is advisable before starting statin therapy. Test for serum creatinine and proteinuria. Conclusions for my health - current risk of CVD is 8% - table 1
- Aspirin is of limited value or unsafe
- Statins are safe and should be taken daily after
- a baseline checkup (total cholesterol, LDL, HDL, Triglycerides, blood pressure, Creatine Kinase, liver transaminase, serum creatinine and proteinuria)
- Statin treatment targets
- 30% reduction in LDL cholesterol (from 3 to 1.9 mmol/l)
- 24% reduction in total cholesterol (from 5.1 to 3.88 mmol/l)
- reduce risk of CVD by 25% - from 1 in 12 (8%) to 1 in 17 (6%) over 10 years - table 2.
- Fibrates or Nicotinic acid treatment targets (after initial statin treatment)
- Reduce CVD risk to 5% (1 in 20) by increasing HDL cholesterol to medium levels (1.34 mmol/l) - table 3
- Reduce CVD risk to 4% (1 in 25) by increasing HDL cholesterol to high levels (1.73 mmol/l) - table 4
- Reduce CVD risk to 3% (1 in 33) by reducing systolic blood pressure from 130 to 108 mmHg by improving diet and increasing exercise - table 5
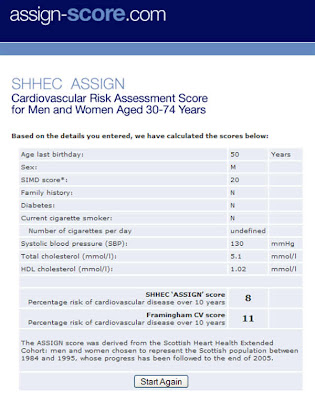 Table 1: Baseline 8% risk
Table 1: Baseline 8% risk 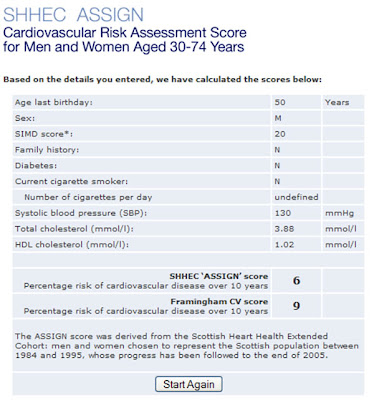 Table 2: 6% risk after Statin treatment
Table 2: 6% risk after Statin treatment 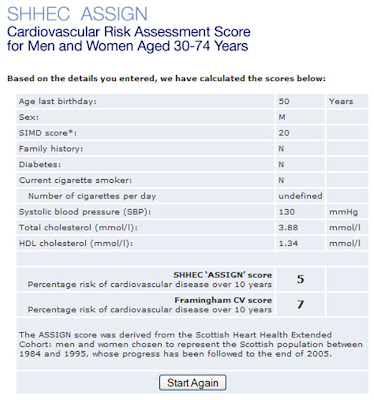 Table 3: 5% risk after treatment to give medium HDL cholesterol levels
Table 3: 5% risk after treatment to give medium HDL cholesterol levels 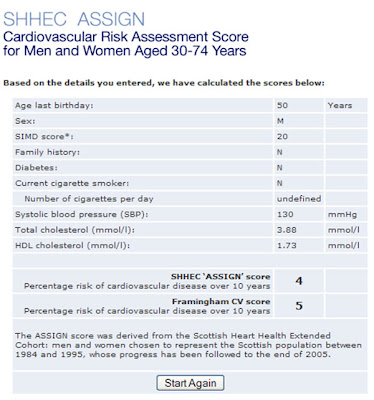 Table 4: 4% risk after treatment to give high HDL cholesterol levels
Table 4: 4% risk after treatment to give high HDL cholesterol levels 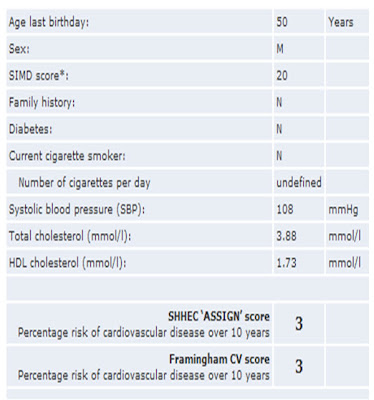
Table 5: 3% risk after treatment to give low blood pressure
No comments:
Post a Comment